Is a minimum unit price an effective and cost-effective policy for reducing alcohol-related harm?
Globally, alcohol is ranked as the seventh leading risk factor for ill-health, disability and death among all ages, increasing steadily between 1990 and 2016 (Global Burden of Disease [GBD], 2016). In the United Kingdom (UK), alcohol is the fourth leading cause among all ages, and among those aged 15-49 is the second, accounting for 5.8% of all disability adjusted life years (DALYs). The economic burden of alcohol is estimated to be as much as £52 billion annually (Rehm et al., 2009).
The burden of alcohol related harm is wide ranging, impacting not only on the drinkers themselves, but those around them (Laslett et al., 2010). Alcohol related harm relates to the dose and frequency of consumption, though mostly harm increases in a dose-response fashion, with greater levels of consumption being associated with greater levels of harm (World Health Organization [WHO], 2014). Patterns of drinking equate to types of harm, for example single occasions of high volume consumption increase risk of injury (Taylor et al., 2010) and heart arrhythmia (Voskoboinik et al., 2016), while lower levels of frequent consumption increase the risk of hypertension (Husain et al., 2014), and regular heavy drinking is associated with alcohol-related liver disease (Rehm et al., 2010). Alcohol interacts with other risky behaviours in a synergistic way, such that the sum of the two risks for a condition is less than the observed level of risk – this is true for smoking and drinking and head and neck cancers (Hart et al., 2010), and drinking and excess weight for liver disease (Liu et al., 2010).
The harm caused by alcohol is not isolated to health. Families are affected by alcohol due to relationship breakdown (Barnow et al., 2002), intimate partner violence (WHO, 2012), and child abuse and neglect (Magura and Laudet, 1996). Alcohol is also an important factor in criminal behavior (Johnston et al., 2012), involved in almost half of all violent incidents (Kroner et al., 2007). Alcohol also impacts negatively on factors relating to the workplace, associated with higher levels of unemployment (Henkel, 2011), absenteeism and sickness and loss of productivity (Dale and Livingston, 2010). Taken together, it is clear the public health burden of alcohol is substantial, and effective and cost-effective public health policies to reduce its burden are required.
A range of alcohol control policies have been designed with the central aim of reducing alcohol related harm as follows (Burton et al., 2017):
- Taxation and price regulation
- Regulating marketing
- Reducing availability
- Managing the drinking environment
- Reducing drink-driving
- The provision of information
- Treatment and brief interventions delivered in the health service
The WHO recognises a number of ‘best buys’ regarding policies to reduce alcohol related harm including taxation and price regulation, regulating marketing, and reducing availability (WHO, 2014). The evidence contained within other academic reviews mirror these recommendations, often suggesting taxation and price regulation to be among the most effective and cost-effective policies (Burton et al., 2017, Babor et al., 2003, Anderson et al., 2009). These policies include increases in taxation, bans on the sale of alcohol below cost (operationalised as the cost of duty added with value added tax [VAT]), bans on multi-buys (such as buy one get one free), and the implementation of a minimum unit price (MUP) for alcohol (Burton et al., 2017). This essay focuses on the effectiveness and cost-effectiveness of MUP, specifically within a UK context.
Evidence from systematic reviews and meta-analyses including over 1,000 estimates demonstrate that the price of alcohol is strongly related to levels of alcohol consumption (Wagenaar et al., 2009) and alcohol related harm (Wagenaar et al., 2010). As the price of alcohol increases, the amount consumed decreases. While there are differences across groups, such as sex, age, and socioeconomic status, and product type, such as beer or wine, this price-consumption relationship remains (Meng et al., 2014). This evidence forms the basis for the mechanism of action of a MUP since the affordability (a composite measure of income and price) is a determinant of alcohol consumption.
If you need assistance with writing your assignment, our professional Assignment Writing Service is here to help!
Find out moreIn essence, a MUP is a legally mandated minimum price for a unit of alcohol, below which it cannot be sold. Various levels have been proposed between 45p and 60p, though the most recent modelling relates to 60p and will be presented herein (Angus and Ally, 2015, Angus et al., 2015, Holmes et al., 2014, Meier et al., 2016). Figure 1 shows the impact of a 60p MUP on alcohol deaths and hospital admissions using the narrow and broad measure (briefly the narrow measure maps onto acute health conditions whereas the broad maps onto chronic conditions) (Angus and Ally, 2015).
Figure 1: The estimated impact of a 60p MUP on alcohol deaths and hospital admissions in England cumulatively at 5 years following implementation (Angus and Ally, 2015)

Clearly, the modelling estimates a MUP to have a large impact on alcohol related harm. Modelling the impact of this policy in an Australian context revealed similar findings (Sharma et al., 2016). This evidence is further supported by natural experiments evaluating the impact of a MUP in Canadian provinces, where a 32% reduction in alcohol related mortality was observed within one year of the policy’s implementation (Stockwell et al., 2012). Sizeable reductions were also observed for alcohol related hospital admissions (Stockwell et al., 2013), and alcohol related crime and drink driving offences (Zhao et al., 2013).
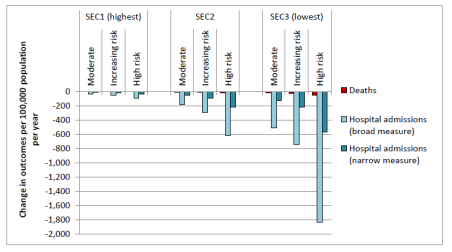
Importantly, while increases in taxation affects all alcohol wherever it is sold, and therefore all consumer groups, a MUP is estimated to proportionally affect heavier drinkers to a greater extent (Figure 2) (Angus and Ally, 2015). This should be viewed positively, since heavier drinkers experience greater levels of alcohol related harm, and moderate drinkers are less affected by this policy.
Figure 2: Estimated impact of a 60p MUP on alcohol deaths and hospital admissions by drinker-type per 100,000 population in England (Angus and Ally, 2015)

Modelling for a 60p MUP also shows that the impact of the policy is not equally distributed across socioeconomic groups (Figure 3) (Angus and Ally, 2015). This suggests that a MUP has the potential to decrease health inequalities, since alcohol related harm is concentrated among the lowest socioeconomic groups. Indeed, of over 1 million hospital admissions annually, around half of all admissions occur in the lowest three socioeconomic groups (Burton et al., 2017).
Figure 3: The estimated impact of a 60p MUP on socioeconomic groups in England, cumulatively at 5 years following policy implementation (Angus and Ally, 2015)
It could be suggested that a MUP is ‘unfair’ or ‘regressive’ on lower socioeconomic groups, since they typically buy the cheapest alcohol and therefore experience the highest consumer price increases. Nonetheless, if the policy is viewed as one which disproportionately benefits the most marginalised, then the policy can be seen as positive with regards to health inequalities. Neither of these are correct, and instead relate to an individual’s ideology, or how they personally choose to view the impact of the policy.
Because of the impact of MUP on heavy drinkers and those experiencing the greatest amount of harm, the policy may be viewed as being targeted, even though it is applied at the population level. As such, a MUP represents a unique policy in that it is simultaneously a universal and targeted approach to public health.
Regarding health economic evidence for the policy, implementing a MUP has a low implementation cost – essentially the costs associated with usual legislative processes – and increases revenue to the Exchequer through increased VAT by £380m making it a cost-effective policy (Angus and Ally, 2015). It should be noted that for taxation, all increased revenue goes to the Exchequer – in the order of £1.8 billion over five years, whereas for a MUP, the increased revenue largely goes to retailers (Burton et al., 2017). In the Canadian provinces where the sale of alcohol is monopolised (state owned), the raised revenue from a MUP goes to the state (Stockwell et al., 2015). Currently, the way the European Union (EU) directive is laid out precludes a form of MUP in the UK where the revenue could go to the Exchequer (Burton et al., 2017).
If you need assistance with writing your assignment, our professional Assignment Writing Service is here to help!
Find out moreAfter five years of delay due to a legal opposition led by the Scotch Whisky Association, the UK Supreme Court officially ruled that the implementation of a MUP is legal in the UK under the EU directive (UK Supreme Court, 2017). As such, Scotland have implemented a 50p MUP from 1st May 2018. Wales are currently seeking devolved powers to implement a MUP, and Ireland are trying to pass legislation for a MUP set at €1 per unit of alcohol sold. It is unclear whether Northern Ireland will follow suit. England stands alone as the only country within the UK to actively choose not to implement the policy. This represents one of the single most important natural experiments in the UK’s contemporary alcohol policy for decades, and provides an important opportunity for evaluation.
References
Anderson, P., Chisholm, D. & Fuhr, D. C. 2009. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. The Lancet, 373, 2234-2246.
Angus, C. & Ally, A. 2015. Modelling the potential impact of duty policies using the Sheffield Alcohol Policy Model Version 3.
Angus, C., Gillespie, D., Ally, A. & Brennan, A. 2015. Modelling the impact of Minimum Unit Price and Identification and Brief Advice policies using the Sheffield Alcohol Policy Model Version 3.
Babor, T., Cactano, R., Casswell, S., Edwards, G., Giesbrecht, N., Graham, K., Grube, J., Gruenewald, P., Hill, L. & Holder, H. 2003. Alcohol: No ordinary commodity. A summary of the book. Addiction, 98.
Barnow, S., Schuckit, M. A., Lucht, M., John, U. & Freyberger, H. J. 2002. The importance of a positive family history of alcoholism, parental rejection and emotional warmth, behavioral problems and peer substance use for alcohol problems in teenagers: a path analysis. Journal of studies on alcohol, 63, 305-315.
Burton, R., Henn, C., Lavoie, D., O'connor, R., Perkins, C., Sweeney, K., Greaves, F., Ferguson, B., Beynon, C. & Belloni, A. 2017. A rapid evidence review of the effectiveness and cost-effectiveness of alcohol control policies: an English perspective. The Lancet, 389, 1558-1580.
Dale, C. E. & Livingston, M. J. 2010. The burden of alcohol drinking on co-workers in the Australian workplace. Med J Aust, 193, 138-40.
Global Burden of Disease 2016. Global Burden of Disease Visualisation Tool.
Hart, C. L., Smith, G. D., Gruer, L. & Watt, G. C. 2010. The combined effect of smoking tobacco and drinking alcohol on cause-specific mortality: a 30 year cohort study. BMC Public Health, 10, 789.
Henkel, D. 2011. Unemployment and substance use: a review of the literature (1990-2010). Current drug abuse reviews, 4, 4-27.
Holmes, J., Meng, Y., Meier, P. S., Brennan, A., Angus, C., Campbell-Burton, A., Guo, Y., Hill-Mcmanus, D. & Purshouse, R. C. 2014. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: a modelling study. The Lancet, 383, 1655-1664.
Husain, K., Ansari, R. A. & Ferder, L. 2014. Alcohol-induced hypertension: Mechanism and prevention. World journal of cardiology, 6, 245.
Johnston, M. C., Ludbrook, A. & Jaffray, M. A. 2012. Inequalities in the Distribution of the Costs of Alcohol Misuse in Scotland: A Cost of Illness Study. Alcohol and Alcoholism, 47, 725-731.
Kroner, D. G., Mills, J. F. & Morgan, R. D. 2007. Underreporting of crime-related content and the prediction of criminal recidivism among violent offenders. Psychological Services, 4, 85.
Laslett, Catalano, P., Chikritzhs, T., Dale, C., Doran, C., Ferris, J., Jainullabudeen, T., Livingston, M., Matthews, S., Mugavin, J., Room, R., Schlotterlein, M. & Wilkinson, C. 2010. The range and magnitude of alcohol's harm to others.
Liu, B., Balkwill, A., Reeves, G. & Beral, V. 2010. Body mass index and risk of liver cirrhosis in middle aged UK women: prospective study. BMJ, 340.
Magura, S. & Laudet, A. B. 1996. Parental substance abuse and child maltreatment: Review and implications for intervention. Children and Youth Services Review, 18, 193-220.
Meier, P. S., Holmes, J., Angus, C., Ally, A. K., Meng, Y. & Brennan, A. 2016. Estimated effects of different alcohol taxation and price policies on health inequalities: a mathematical modelling study. PLoS Med, 13, e1001963.
Meng, Y., Brennan, A., Purshouse, R., Hill-Mcmanus, D., Angus, C., Holmes, J. & Meier, P. S. 2014. Estimation of own and cross price elasticities of alcohol demand in the UK—A pseudo-panel approach using the Living Costs and Food Survey 2001–2009. Journal of Health Economics, 34, 96-103.
Rehm, J., Mathers, C., Popova, S., Thavorncharoensap, M., Teerawattananon, Y. & Patra, J. 2009. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet, 373, 2223-2233.
Rehm, J., Taylor, B., Mohapatra, S., Irving, H., Baliunas, D., Patra, J. & Roerecke, M. 2010. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta‐analysis. Drug and alcohol review, 29, 437-445.
Sharma, A., Etilé, F. & Sinha, K. 2016. The effect of introducing a minimum price on the distribution of alcohol purchase: a counterfactual analysis. Health economics, 25, 1182-1200.
Stockwell, T., Zhao, J., Giesbrecht, N., Macdonald, S., Thomas, G. & Wettlaufer, A. 2012. The raising of minimum alcohol prices in Saskatchewan, Canada: impacts on consumption and implications for public health. American Journal of Public Health, 102, e103-e110.
Stockwell, T., Zhao, J., Martin, G., Macdonald, S., Vallance, K., Treno, A., Ponicki, W., Tu, A. & Buxton, J. 2013. Minimum alcohol prices and outlet densities in British Columbia, Canada: estimated impacts on alcohol-attributable hospital admissions. American journal of public health, 103, 2014-2020.
Stockwell, T., Zhao, J., Marzell, M., Gruenewald, P. J., Macdonald, S., Ponicki, W. R. & Martin, G. 2015. Relationships between minimum alcohol pricing and crime during the partial privatization of a Canadian government alcohol monopoly. Journal of studies on alcohol and drugs, 76, 628-634.
Taylor, B., Irving, H., Kanteres, F., Room, R., Borges, G., Cherpitel, C., Greenfield, T. & Rehm, J. 2010. The more you drink, the harder you fall: a systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug and alcohol dependence, 110, 108-116.
Uk Supreme Court 2017. Judgement. Scotch Whisky Association and others (Appellants) v The Lord Advocate and another (Respondents) (Scotland).
Voskoboinik, A., Prabhu, S., Ling, L.-H., Kalman, J. M. & Kistler, P. M. 2016. Alcohol and atrial fibrillation: a sobering review. Journal of the American College of Cardiology, 68, 2567-2576.
Wagenaar, A. C., Salois, M. J. & Komro, K. A. 2009. Effects of beverage alcohol price and tax levels on drinking: a meta‐analysis of 1003 estimates from 112 studies. Addiction, 104, 179-190.
Wagenaar, A. C., Tobler, A. L. & Komro, K. A. 2010. Effects of Alcohol Tax and Price Policies on Morbidity and Mortality: A Systematic Review. American Journal of Public Health, 100, 2270-2278.
World Health Organization [WHO]. 2012. Understanding and addressing violence against women. Intimate partner violence.
World Health Organization [WHO]. 2014. Global status report on alcohol and health.
Zhao, J., Stockwell, T., Martin, G., Macdonald, S., Vallance, K., Treno, A., Ponicki, W. R., Tu, A. & Buxton, J. 2013. The relationship between minimum alcohol prices, outlet densities and alcohol‐attributable deaths in British Columbia, 2002–09. Addiction, 108, 1059-1069.
Cite This Work
To export a reference to this article please select a referencing style below: